Practice Policies & Patient Information
Access To Medical Records
Notes on Medical Record Access
Data Protection Act 2018 and GDPR gave individuals the right to their medical records.
Who has the right of Access?
The patient/ A child’s parent/ Someone acting on behalf of patient.
How should the application be made?
Individuals wish to access their medical record should make an application online. The practice may require identify the individual.
How long should application take?
Access should be given within 30 days of application being made. The period can be extended for further two months where requests are complex or numerous.
Fees
Access to medical records is free. However, practice can charge reasonable fee where an individual or body makes repeated request for the same information.
Apply For Access To Medical Records
Anti-Coagulation Records
LumiraDX Care Solutions anti-coagulation clinics data is being moved to INRstar to a Cloud-First technology. Your anti-coagulation clinics data will be continued to be held in England. For further details about how this data is handled, please refer to the notice here. If you have any queries, please contact the practice manager.
General Practice Data for Planning and Research – Data Sharing
For more information about this visit NHS Digital
As of 1st September 2021 your data will be shared with NHS Digital to help improve health, care and services.
Patient data from GP medical records kept by GP practices in England is used every day to improve health, care and services through planning and research, helping to find better treatments and improve patient care. The NHS is introducing an improved way to share this information – called the General Practice Data for Planning and Research data collection.
NHS Digital will collect, analyse, publish and share this patient data to improve health and care services for everyone.
This includes:
- informing and developing health and social care policy
- planning and commissioning health and care services
- taking steps to protect public health (including managing and monitoring the coronavirus pandemic)
- in exceptional circumstances, providing you with individual care
- enabling healthcare and scientific research
Any data that NHS Digital collects will only be used for health and care purposes. It is never shared with marketing or insurance companies.
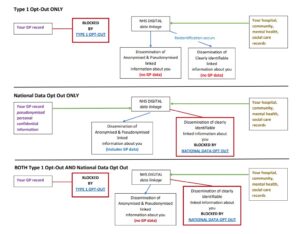
NHS Digital will not collect any patient data for patients who have already registered a Type 1 opt-out in line with current policy. If this changes patients who have registered a Type 1 opt-out will be informed.
If you do not want your patient data shared with NHS Digital, you can register a Type 1 opt-out with us. You can register a Type 1 opt-out at any time. You can also change your mind at any time and withdraw a Type 1 opt-out.
Data sharing with NHS Digital will start on 1st September 2021.
If you have already registered a Type 1 opt-out with your GP practice your data will not be shared with NHS Digital.
If you wish to register a Type 1 opt-out with your GP practice before data sharing starts with NHS Digital, this should be done by completing this form by 24 August 2021 to allow time for processing it.
If you have previously registered a Type 1 opt-out and you would like to withdraw this, you can also use the form to do this.
If you register a Type 1 opt-out after your patient data has already been shared with NHS Digital, no more of your data will be shared with NHS Digital. NHS Digital will however still hold the patient data which was shared with us before you registered the Type 1 opt-out.
If you do not want NHS Digital to share your identifiable patient data with anyone else for purposes beyond your own care, then you can also register a National Data Opt-out (also known as a Type 2 opt out).
What do you need to do?
If you are happy for your data to be shared as above, and you have not previously opted out – you do not need to do anything.
Type 1 OPT-OUT – to stop sharing your details with NHS digital (or to opt back in, if you have previously opted out) – Complete this form
Type 2 OPT-OUT (also known as National Data Opt-out) – if you do not want NHS Digital to share your identifiable patient data with anyone else for purposes beyond your own care (or to opt back in, if you have previously opted out)
You need to, either:
- Call 0300 303 5678
- or complete their online form
As a GP practice WE CANNOT opt you out of Type 2 (National Data Opt-out)
Net GP Earnings
NHS England require that the net earnings of doctors engaged in the practice is publicised and that the required disclosure is shown below.
The average pay for GPs working at Churchill Medical Centre in the last financial year was £81,544 before tax and National Insurance. This is for 1 full time GP and 11 part time GPs who worked in the practice for more than six months.
However it should be noted that the prescribed method for calculating earnings is potentially misleading because it takes no account of how much time doctors working in the practice and should not be used for any judgement about GP earnings, nor to make comparisons with other practices.
Privacy Notices
Churchill Medical Centre has taken measure to comply with the new General Data protection Regulation (‘GDPR’, Regulation (EU) 2016/679) which has come into effect on the 25th May 2018.
Privacy Notice
How we use your medical records. Important information for patients
- This practice handles medical records in-line with laws on data protection and confidentiality.
- We share medical records with those who are involved in providing you with care and treatment.
- In some circumstances we will also share medical records for medical research, for example to find out more about why people get ill.
- We share information when the law requires us to do so, for example, to prevent infectious diseases from spreading or to check the care being provided to you is safe.
- Calls are recorded for training and monitoring purposes.
- You have the right to be given a copy of your medical record.
- You have the right to object to your medical records being shared with those who provide you with care.
- You have the right to object to your information being used for medical research and to plan health services.
- You have the right to have any mistakes corrected and to complain to the Information Commissioner’s Office. Please see the practice privacy notice on the website or speak to a member of staff for more information about your rights.
Data Protection and Call Recording Notice
At Churchill Medical Centre, we are committed to providing the highest quality of care to our patients. As part of our continuous efforts to enhance our services, please be advised that calls made to and from our practice may be recorded for training and quality assurance purposes.
The recordings are securely stored and accessible only to authorised personnel. These recordings assist us in ensuring that our team consistently maintains the highest standards of professionalism, accuracy, and patient care. Additionally, they help us identify areas for improvement and enhance the training of our staff.
Rest assured that the information shared during these calls is treated with the utmost confidentiality and in accordance with data protection regulations. Personal information is carefully handled, and any recorded data is subject to the same stringent privacy and security measures as other patient information.
If you have any concerns about the recording of your calls or the protection of your data, please feel free to discuss this with our team. Your privacy and peace of mind are of paramount importance to us, and we are here to address any questions you may have.
How your information is used for medical research and to measure the quality of care
Medical research
Churchill Medical Centre shares information from medical records:
- to support medical research when the law allows us to do so, for example to learn more about why people get ill and what treatments might work best;
- we will also use your medical records to carry out research within the practice.
This is important because:
- the use of information from GP medical records is very useful in developing new treatments and medicines;
- medical researchers use information from medical records to help answer important questions about illnesses and disease so that improvements can be made to the care and treatment patients receive.
We share information with the following medical research organisations with your explicit consent or when the law allows:
- CPRD – Clinical Practice Research Datalink
- National Diabetes Audit
- ACR project for patients with diabetes (and/or other conditions)
You have the right to object to your identifiable information being used or shared for medical research purposes. Please speak to the practice if you wish to object.
Checking the quality of care – national clinical audits
Churchill Medical Centre contributes to national clinical audits so that healthcare can be checked and reviewed.
- Information from medical records can help doctors and other healthcare workers measure and check the quality of care which is provided to you.
- The results of the checks or audits can show where hospitals are doing well and where they need to improve.
- The results of the checks or audits are used to recommend improvements to patient care.
- Data are sent to NHS Digital a national body with legal responsibilities to collect data.
- The data will include information about you, such as your NHS Number and date of birth and information about your health which is recorded in coded form – for example the code for diabetes or high blood pressure.
- We will only share your information for national clinical audits or checking purposes when the law allows.
- For more information about national clinical audits see the Healthcare Quality Improvements Partnership website or phone 020 7997 7370.
- You have the right to object to your identifiable information being shared for national clinical audits. Please contact the practice if you wish to object.
We are required by law to provide you with the following information about how we share your information for medical research purposes.
| Data Controller contact details | Churchill Medical Centre 1 Churchill terrace Chingford E4 8DG |
|---|---|
| Data Protection Officer contact details | Dr P J Koczan Tel: 020 8430 7020 |
| Purpose of the processing | Medical research and to check the quality of care which is given to patients (this is called national clinical audit). |
| Lawful basis for processing | The following sections of the GDPR mean that we can use medical records for research and to check the quality of care (national clinical audits) Article 6(1)(e) – ‘processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller’. For medical research: there are two possible Article 9 conditions. Article 9(2)(a) – ‘the data subject has given explicit consent…’ Article 9(2)(j) – ‘processing is necessary for… scientific or historical research purposes or statistical purposes in accordance with Article 89(1) based on Union or Member States law which shall be proportionate to the aim pursued, respect the essence of the right to data protection and provide for suitable and specific measures to safeguard the fundamental rights and interests of the data subject’. To check the quality of care (clinical audit): Article 9(2)(h) – ‘processing is necessary for the purpose of preventative…medicine…the provision of health or social care or treatment or the management of health or social care systems and services…’ |
| Recipient or categories of recipients of the processed data | For medical research the data will be shared with : CPRD – Clinical Practice Research Datalink and National Diabetes Audit |
| Rights to objec and the national data opt-out | You have a right to object under the GDPR and the right to ‘opt-out’ under the national data opt-out model. The national data opt-out model provides an easy way for you to opt-out of: information that identifies you being used or shared for medical research purposes and quality checking or audit purposes. Please contact the practice if you wish to opt-out. To opt-out of your identifiable information being shared for medical research or to find out more about your optout choices please go to NHS Digital’s website phone number for general enquires 0300 303 5678 |
| Right to access and correct |
|
| Retention period | GP medical records will be kept in line with the law and national guidance. Information on how long records are kept can be found by clicking here or speak to the practice. |
| Right to complain | You have the right to complain to the Information Commissioner’s Office. If you wish to complain please click here to visit the website or call the helpline 0303 123 1113 |
Legal Requirements For Data Sharing
How your information is shared so that this practice can meet legal requirements
The law requires Churchill Medical Centre to share information from your medical records in certain circumstances. Information is shared so that the NHS or Public Health England can, for example:
- plan and manage services;
- check that the care being provided is safe;
- prevent infectious diseases from spreading.
We will share information with NHS Digital, the Care Quality Commission and local health protection team (or Public Health England) when the law requires us to do so. Please see below for more information.
We must also share your information if a court of law orders us to do so.
NHS Digital
NHS Digital is a national body which has legal responsibilities to collect information about health and social care services.
- It collects information from across the NHS in England and provides reports on how the NHS is performing. These reports help to plan and improve services to patients.
- This practice must comply with the law and will send data to NHS Digital, for example, when it is told to do so by the Secretary of State for Health or NHS England under the Health and Social Care Act 2012.
- More information about NHS Digital and how it uses information can be found on their website
Care Quality Commission (CQC)
- The CQC regulates health and social care services to ensure that safe care is provided.
- The law says that we must report certain serious events to the CQC, for example, when patient safety has been put at risk.
- For more information about the CQC please visit their website
Public Health
- The law requires us to share data for public health reasons, for example to prevent the spread of infectious diseases or other diseases which threaten the health of the population.
- We will report the relevant information to local health protection team or Public Health England.
- For more information about Public Health England and disease reporting please visit their website
We are required by law to provide you with the following information about how we handle your information and our legal obligations to share data.
| Data Controller contact details | Churchill Medical Centre 1 Churchill Terrace Chingford E4 8DG |
|---|---|
| Data Protection Officer contact details | Dr P Koczan Tel: 020 8430 7020 |
| Purpose of the processing | Compliance with legal obligations or court order. |
| Lawful basis for processing | The following sections of the GDPR mean that we can share information when the law tells us to. Article 6(1)(c) – ‘processing is necessary for compliance with a legal obligation to which the controller is subject…’ Article 9(2)(h) – ‘processing is necessary for the purpose of preventative…medicine…the provision of health or social care or treatment or the management of health or social care systems and services…’ |
| Recipient or categories of recipients of the processed data |
|
| Rights to object and the national data opt-out | There are very limited rights to object when the law requires information to be shared but government policy allows some rights of objection as set out below. NHS Digital
To opt-out or to find out more about your opt-out choices please go to NHS Digital’s website
|
| Right to access and correct |
|
| Retention period | GP medical records will be kept in line with the law and national guidance. Information on how long records are kept can be found by clicking here or speak to the practice. |
| Right to complain | You have the right to complain to the Information Commissioner’s Office. If you wish to complain please visit their website or call the helpline 0303 123 1113 |
National Screening Programme
The NHS provides national screening programmes so that certain diseases can be detected at an early stage.
- These screening programmes include bowel cancer, breast cancer, cervical cancer, aortic aneurysms and a diabetic eye screening service.
- The law allows us to share your contact information with Public Health England so that you can be invited to the relevant screening programme.
- More information can be found on the Government’s website or speak to the practice
We are required by law to provide you with the following information about how we handle your information in relation to our legal obligations to share data.
| Data Controller contact details | Churchill Medical Centre 1 Churchill Terrace Chingford E4 8DG |
|---|---|
| Data Protection Officer contact details | Dr P Koczan Tel: 020 8430 7020 |
| Purpose of the processing |
|
| Lawful basis for processing | The following sections of the GDPR allow us to contact patients for screening. Article 6(1)(e) – ‘processing is necessary…in the exercise of official authority vested in the controller…’’ Article 9(2)(h) – ‘processing is necessary for the purpose of preventative…medicine…the provision of health or social care or treatment or the management of health or social care systems and services…’ |
| Recipient or categories of recipients of the processed data | The data will be shared with:
|
| Rights to object | For national screening programmes: you can opt so that you no longer receive an invitation to a screening programme. See the government’s website or speak to your practice. |
| Right to access and correct |
|
| Retention period | GP medical records will be kept in line with the law and national guidance. Information on how long records can be kept can be found on the NHS Digital Website or speak to the practice. |
| Right to complain | You have the right to complain to the Information Commissioner’s Office. If you wish to complain please go to the ICO website or call the helpline 0303 123 1113 |
| Data we get from other organisations | We receive information about your health from other organisations who are involved in providing you with health and social care. For example, if you go to hospital for treatment or an operation the hospital will send us a letter to let us know what happens. This means your GP medical record is kept up-to date when you receive care from other parts of the health service. |
Safe Surgeries New Patient Registration Policy
Introduction
Patient registration is determined by the provisions of the practice GMS or PMS contract and terms of service. This policy is based on the NHS England Standard General Medical Service Contract, the General Medical Services Contract Regulations, Primary Medical Care Policy and Guidance Manual (PGM) and CQC guidance.
Practices are assumed to have open lists unless they have complied with the procedures for list closure as detailed in the General Medical Services Contracts Regulations. Where a practice has an open list it is required to:
- accept the registration of a new patient unless it has fair and reasonable grounds for not doing so
- accept allocations by the ICB to its list.
The practice can formally close their list to new patients by requesting permission from its commissioner. Formal list closure lasts between three to twelve months, and cannot last less than three months.
In some cases, it may be possible to request an ‘informal’ or ‘temporary’ list closure, lasting less than three months, for example where staffing difficulties result in suspension of registrations being necessary. GMS and PMS contracts do not allow for these types of list closures, but taking into consideration possible risk to patient care, the practice can discuss these circumstances with their commissioner, who can either provide further support or approve temporary closure, if appropriate.
Patient Choice of GP Practice
From 5th January 2015, all GP practices in England are free to register new patients who live outside their practice boundary area, without obligation to provide home visits. This will provide patients with greater choice and aims to improve the quality of access to GP services.
Patients may wish to register as out of area patients to:
- register with a practice in more convenient locations, such as a practice near their work or closer to their children’s schools, or they reside within the area during the week, but their permanent address is in another area
- stay registered with their current GP if they have moved home but do not want to change GP
- register in an area with better access to services
These new arrangements are voluntary for GP practices. If the practice has no capacity at the time, or feels it is not clinically appropriate or practical for patients to be registered so far away from their home address, they can still refuse registration for out of area patients. The practice should explain their reason for refusing registration to patients. When registration is refused, patient choice is not fully realised.
New Patient Acceptance/Refusal
New patients should submit a New Patient Registration/Health Questionnaire and the new style GMS1 Form.
The practice will accept patients onto its list while it remains “open”. If the list is closed, the practice will only accept registrations of immediate family members of patients who are already registered and only if such relatives reside permanently at the registered patient’s address.
For patients who self-declare that they hold either a non-UK issued EHIC, PRC or S1 form, the practice is required to manually record this information in the patient’s medical record and then send a copy of the GMS1 form to NHS Digital – NHSDigital-EHIC@nhs.net (for Non-UK issued EHIC/PRC details) or the Department of Work and Pensions (DWP) overseas.healthcare@dwp.gsi.gov.uk (for S1 forms).
Patients will not be unreasonably refused registration. This includes refusal based on:
- Medical condition
- Race
- Social class
- Gender or sexual orientation
- Disability
- Age
- Immigration status
- Religious group or religious beliefs
- Political beliefs
- Appearance or lifestyle
The practice will, however, refuse registration if the commissioner has agreed that they can close their list to new patients. The practice can also refuse registration (subject to a partners’ discussion and agreement) if:
- The patient has been previously removed from the list
- The patient has a known history of violence
- The patient lives outside the practice boundary
- If they have other reasonable grounds
The reason for refusal will be in writing and recorded in a permanent record for that purpose. This excludes temporary residents, where no record is necessary. The permanent record will consist of the original GMS1 registration form endorsed with the reason for refusal, together with a copy of the refusal letter, filed in surname order. Where a GMS1 has not been completed, a “dummy” GMS1 will be prepared and filed. The record is subject to inspection by the ICB, who may require the practice to justify a refusal to register.
ID and Proof of Address
There is no regulatory requirement to prove identity, address, immigration status or the provision of an NHS number in order to register. ID and/or proof of address can be requested to assist with the administrative process, but the practice must apply the same process for requesting documents to all patients requesting registration equally. The majority of patients will not find it difficult to produce documents.
However, there will be some patients who do live in the practice area, but are legitimately unable to produce any of the listed documentation. Examples include:
- People fleeing domestic abuse staying with friends, family or in a shelter
- People living on a boat, in unstable accommodation or street homeless
- People staying long term with friends but who aren’t receiving bills
- People working in exploitative situations whose employer has taken their documents
- People who have submitted their documents to the Home Office as part of an application
- People trafficked into the country who had their documents taken on arrival
- Children born in the UK to parents without documentation.
Reasonable exceptions need to be considered and the individual registered with sensitivity to their situation. As there is no requirement under the regulations to produce identity or residence information, the patient MUST be registered on application unless the practice has reasonable grounds to decline. Lack of ID/proof of residence would not be considered reasonable grounds to refuse to register a patient and access to appointments should not be withheld in these circumstances. If a patient cannot produce any supportive documentation but states that they reside within the practice boundary then practices should accept the registration.
Where necessary, (e.g. homeless patients), the practice may use the practice address to register the patient, putting CO (care of) at the start of the address (as per CQC and PCSE advice). If possible, the practice should try to ensure they have a way of contacting the patient if they need to (for example with test results).
If a practice suspects a patient of fraud (such as using fake ID) then they should register and treat the patient but hand the matter over to the NHS Counter Fraud Authority (NHSCFA).
Access to online services
It is important to note that whilst there is no requirement for ID when initially registering at this organisation, this should not be confused with those patients that wish to have access to online services. Should any patient request online access, then full identification is required and the process should be followed as detailed within the Access to online services policy.
Temporary Residents
If a patient is resident in the practice area for more than 24 hours, but less than three months, they should be offered the option of registering as a temporary patient. In some cases (e.g. someone housed in temporary accommodation) a prospective patient may not know how long they will reside in the area.
Please note: If there is uncertainty around the length of time a patient will reside in the practice area, NHS England advises that the patient should be registered as a permanent patient. For example, asylum seekers residing in Home Office accommodation should be registered as permanent patients.
Emergency Treatment
All GP practices have a contractual duty to provide emergency treatment and immediately necessary treatment free of charge for up to 14 days. This applies to any person within their practice area who:
- Has been refused application for inclusion in the practice’s list of patients
- Is not registered with another provider of essential services
- Has had their application for acceptance as temporary resident rejected
Immediately necessary treatment in relation to people who are visiting England should be viewed as treatment of new and pre-existing conditions that have become worse during their stay. This is subject to the GP’s clinical judgement.
Support and Additional Needs
If a prospective patient requires additional support in order to register, the practice will do its best to accommodate this. This includes (but is not limited to):
- Walking them through the registration process in a more private area of the practice
- Using a translator/ interpreter
- Noting any accessibility requirements on the patient’s record so that the practice team is aware and can support them as necessary.
Once the patient is registered, the patient may benefit from other forms of support, including but not limited to:
- Provision of double appointments
- Reducing/ increasing prescription duration as necessary
- Promoting clear boundaries for consultations
- Providing fast access to a named GP
- Waiving normal charges for housing letters or medical reports
Ensuring services are accessible to everyone who needs them is mandatory. This includes following the Accessible Information Standard and provision of interpreting and translation services.
Registering Vulnerable Groups
Children
If a child under the age of 16 attempts to register alone, or with an adult who does not have parental responsibility for the child, the safeguarding lead should be informed.
It is recommended that the GP practice gains assurance by:
- Obtaining proof of identity for each child registering (e.g. a passport, or birth certificate). If a child does not have any form of ID, this should not prevent them from being registered. In this case, register the child, but ensure that the safeguarding lead is made aware of the registration.
- Ensuring that an adult with parental responsibility is present at registration (and that they can prove parental responsibility).
- Offering a child a new patient health check
- Obtaining supporting documentation from other official sources (e.g. previous GP, social workers etc).
Where any doubt exists, the GP surgery’s safeguarding lead is to be informed and appropriate actions taken.
People with Insecure Immigration Status
Everyone in England, regardless of their immigration status, is entitled to free primary care and to register with a GP. This includes temporary visitors/ tourists, asylum seekers, refugees and other vulnerable migrants. When registering a patient, do not ask about their immigration status, or to see proof of it. People seeking asylum should be registered as permanent patients.
The GMS1 registration form includes supplementary questions about immigration status. These questions are optional – patients do not have to complete this section if they do not want to and this should be communicated clearly to patients. If a patient does opt to complete this section, they should not be asked to provide proof for the information they have provided.
People Experiencing Homelessness
Individuals experiencing homelessness, those without a fixed address, or afraid to share their address, should be registered under either:
- an address of their choosing (e.g. a friend’s address, religious institution, or community centre). Advise the patient that they may receive confidential medical letters to this address, and that they should have the occupiers consent
- under the practice address. When registering the patient, enter the full address, including postcode for the GP practice, putting ‘Care of’ at the start of the address. Writing ‘no fixed abode’ in any field will cause
- the registration request to be rejected.
Ensure that patients are advised to regularly check for post at the address they are registered at, so as not to miss any important medical correspondence (e.g. secondary care appointments).
Duty to refer
The Homelessness Reduction Act (2017) came into force in 2018. It places renewed emphasis on homelessness prevention. Section 10 requires public authorities in England to notify a local housing authority (LHA) of service users they think may be homeless or at risk of becoming homeless.
This statutory duty to refer applies to:
- NHS organisations that provide inpatient care
- emergency departments
- urgent treatment centres.
It is not mandatory for primary care providers. However, it is still beneficial for GP practices to refer patients who are homeless, or are at risk of becoming homeless, to a local housing authority for further support.
Referrals must include:
- the service user name
- their contact details and
- an agreed reason for referring the user.
You can refer without consent to safeguard children and vulnerable adults. Guidance on the duty to refer can be found here.
Patients About to be Released from Prison
The process for registering patients prior to their release from the “secure residential estate” which includes prison, immigration removal centres, young offender institutions or secure training centres, is outlined here.
Veterans
Ex-service personnel or reservists will be provided with copies of their medical records by DPHC (Defence Primary Health Care) on leaving the Armed Forces and becoming a veteran. These records should be given to their new GP practice on registering.
Armed Forces veterans are entitled to priority treatment if their injury or condition came about because of their service (subject to clinical need). This is regardless of whether they receive a war pension. Further guidance can be found here and here.
When registering veterans, the following SNOMED code should be entered at the time of registration: Military veteran SCTID: 753651000000107. Having this code will enable access to specialist care or charity support as necessary for the patient.
Mental Capacity Act
If a person is unable to register because they are unable to make decisions about their care, registration can be done by:
- A relative
- The main carer
- A lasting power of attorney
- A person appointed by a court under the Mental Capacity Act
NHS Health Checks and New Patient Health Checks
All newly registered patients should be offered a New Patient Health Check. Some patients may also be entitled to an NHS Health Check. Please refer to the health check policy for further guidance.
Please also see below patient health questionnaires for people seeking asylum and refugees which can be shared during registration to improve efficiency and effectiveness of New Patient Health Checks.
Further Resources and Guidance
NHS guidance:
- How to register with a GP surgery
- Asylum seeker and refugee one-page registration guide
- Primary Medical Care Policy and Guidance Manual (PGM)
BMA support:
- Guidance on patient registration
- Toolkit for asylum seekers and refugees
PCSE support:
- PCSE guidance on registration
- PCSE contact details and enquiries form
CQC guidance:
- Registration mythbusters
- Registration of migrants, asylum seekers and refugees
- People experiencing homelessness
OHID
- Migrant Health Guide
Doctors of the World
- Safe Surgeries network
- Patient health questionnaires for refugees and people seeking asylum
Safe Surgeries New Patient Registration Policy
Introduction
Patient registration is determined by the provisions of the practice GMS or PMS contract and terms of service. This policy is based on the NHS England Standard General Medical Service Contract, the General Medical Services Contract Regulations, Primary Medical Care Policy and Guidance Manual (PGM) and CQC guidance.
Practices are assumed to have open lists unless they have complied with the procedures for list closure as detailed in the General Medical Services Contracts Regulations. Where a practice has an open list it is required to:
- accept the registration of a new patient unless it has fair and reasonable grounds for not doing so
- accept allocations by the ICB to its list.
The practice can formally close their list to new patients by requesting permission from its commissioner. Formal list closure lasts between three to twelve months, and cannot last less than three months.
In some cases, it may be possible to request an ‘informal’ or ‘temporary’ list closure, lasting less than three months, for example where staffing difficulties result in suspension of registrations being necessary. GMS and PMS contracts do not allow for these types of list closures, but taking into consideration possible risk to patient care, the practice can discuss these circumstances with their commissioner, who can either provide further support or approve temporary closure, if appropriate.
Patient Choice of GP Practice
From 5th January 2015, all GP practices in England are free to register new patients who live outside their practice boundary area, without obligation to provide home visits. This will provide patients with greater choice and aims to improve the quality of access to GP services.
Patients may wish to register as out of area patients to:
- register with a practice in more convenient locations, such as a practice near their work or closer to their children’s schools, or they reside within the area during the week, but their permanent address is in another area
- stay registered with their current GP if they have moved home but do not want to change GP
- register in an area with better access to services
These new arrangements are voluntary for GP practices. If the practice has no capacity at the time, or feels it is not clinically appropriate or practical for patients to be registered so far away from their home address, they can still refuse registration for out of area patients. The practice should explain their reason for refusing registration to patients. When registration is refused, patient choice is not fully realised.
New Patient Acceptance/Refusal
New patients should submit a New Patient Registration/Health Questionnaire and the new style GMS1 Form.
The practice will accept patients onto its list while it remains “open”. If the list is closed, the practice will only accept registrations of immediate family members of patients who are already registered and only if such relatives reside permanently at the registered patient’s address.
For patients who self-declare that they hold either a non-UK issued EHIC, PRC or S1 form, the practice is required to manually record this information in the patient’s medical record and then send a copy of the GMS1 form to NHS Digital – NHSDigital-EHIC@nhs.net (for Non-UK issued EHIC/PRC details) or the Department of Work and Pensions (DWP) overseas.healthcare@dwp.gsi.gov.uk (for S1 forms).
Patients will not be unreasonably refused registration. This includes refusal based on:
- Medical condition
- Race
- Social class
- Gender or sexual orientation
- Disability
- Age
- Immigration status
- Religious group or religious beliefs
- Political beliefs
- Appearance or lifestyle
The practice will, however, refuse registration if the commissioner has agreed that they can close their list to new patients. The practice can also refuse registration (subject to a partners’ discussion and agreement) if:
- The patient has been previously removed from the list
- The patient has a known history of violence
- The patient lives outside the practice boundary
- If they have other reasonable grounds
The reason for refusal will be in writing and recorded in a permanent record for that purpose. This excludes temporary residents, where no record is necessary. The permanent record will consist of the original GMS1 registration form endorsed with the reason for refusal, together with a copy of the refusal letter, filed in surname order. Where a GMS1 has not been completed, a “dummy” GMS1 will be prepared and filed. The record is subject to inspection by the ICB, who may require the practice to justify a refusal to register.
ID and Proof of Address
There is no regulatory requirement to prove identity, address, immigration status or the provision of an NHS number in order to register. ID and/or proof of address can be requested to assist with the administrative process, but the practice must apply the same process for requesting documents to all patients requesting registration equally. The majority of patients will not find it difficult to produce documents.
However, there will be some patients who do live in the practice area, but are legitimately unable to produce any of the listed documentation. Examples include:
- People fleeing domestic abuse staying with friends, family or in a shelter
- People living on a boat, in unstable accommodation or street homeless
- People staying long term with friends but who aren’t receiving bills
- People working in exploitative situations whose employer has taken their documents
- People who have submitted their documents to the Home Office as part of an application
- People trafficked into the country who had their documents taken on arrival
- Children born in the UK to parents without documentation.
Reasonable exceptions need to be considered and the individual registered with sensitivity to their situation. As there is no requirement under the regulations to produce identity or residence information, the patient MUST be registered on application unless the practice has reasonable grounds to decline. Lack of ID/proof of residence would not be considered reasonable grounds to refuse to register a patient and access to appointments should not be withheld in these circumstances. If a patient cannot produce any supportive documentation but states that they reside within the practice boundary then practices should accept the registration.
Where necessary, (e.g. homeless patients), the practice may use the practice address to register the patient, putting CO (care of) at the start of the address (as per CQC and PCSE advice). If possible, the practice should try to ensure they have a way of contacting the patient if they need to (for example with test results).
If a practice suspects a patient of fraud (such as using fake ID) then they should register and treat the patient but hand the matter over to the NHS Counter Fraud Authority (NHSCFA).
Access to online services
It is important to note that whilst there is no requirement for ID when initially registering at this organisation, this should not be confused with those patients that wish to have access to online services. Should any patient request online access, then full identification is required and the process should be followed as detailed within the Access to online services policy.
Temporary Residents
If a patient is resident in the practice area for more than 24 hours, but less than three months, they should be offered the option of registering as a temporary patient. In some cases (e.g. someone housed in temporary accommodation) a prospective patient may not know how long they will reside in the area.
Please note: If there is uncertainty around the length of time a patient will reside in the practice area, NHS England advises that the patient should be registered as a permanent patient. For example, asylum seekers residing in Home Office accommodation should be registered as permanent patients.
Emergency Treatment
All GP practices have a contractual duty to provide emergency treatment and immediately necessary treatment free of charge for up to 14 days. This applies to any person within their practice area who:
- Has been refused application for inclusion in the practice’s list of patients
- Is not registered with another provider of essential services
- Has had their application for acceptance as temporary resident rejected
Immediately necessary treatment in relation to people who are visiting England should be viewed as treatment of new and pre-existing conditions that have become worse during their stay. This is subject to the GP’s clinical judgement.
Support and Additional Needs
If a prospective patient requires additional support in order to register, the practice will do its best to accommodate this. This includes (but is not limited to):
- Walking them through the registration process in a more private area of the practice
- Using a translator/ interpreter
- Noting any accessibility requirements on the patient’s record so that the practice team is aware and can support them as necessary.
Once the patient is registered, the patient may benefit from other forms of support, including but not limited to:
- Provision of double appointments
- Reducing/ increasing prescription duration as necessary
- Promoting clear boundaries for consultations
- Providing fast access to a named GP
- Waiving normal charges for housing letters or medical reports
Ensuring services are accessible to everyone who needs them is mandatory. This includes following the Accessible Information Standard and provision of interpreting and translation services.
Registering Vulnerable Groups
Children
If a child under the age of 16 attempts to register alone, or with an adult who does not have parental responsibility for the child, the safeguarding lead should be informed.
It is recommended that the GP practice gains assurance by:
- Obtaining proof of identity for each child registering (e.g. a passport, or birth certificate). If a child does not have any form of ID, this should not prevent them from being registered. In this case, register the child, but ensure that the safeguarding lead is made aware of the registration.
- Ensuring that an adult with parental responsibility is present at registration (and that they can prove parental responsibility).
- Offering a child a new patient health check
- Obtaining supporting documentation from other official sources (e.g. previous GP, social workers etc).
Where any doubt exists, the GP surgery’s safeguarding lead is to be informed and appropriate actions taken.
People with Insecure Immigration Status
Everyone in England, regardless of their immigration status, is entitled to free primary care and to register with a GP. This includes temporary visitors/ tourists, asylum seekers, refugees and other vulnerable migrants. When registering a patient, do not ask about their immigration status, or to see proof of it. People seeking asylum should be registered as permanent patients.
The GMS1 registration form includes supplementary questions about immigration status. These questions are optional – patients do not have to complete this section if they do not want to and this should be communicated clearly to patients. If a patient does opt to complete this section, they should not be asked to provide proof for the information they have provided.
People Experiencing Homelessness
Individuals experiencing homelessness, those without a fixed address, or afraid to share their address, should be registered under either:
- an address of their choosing (e.g. a friend’s address, religious institution, or community centre). Advise the patient that they may receive confidential medical letters to this address, and that they should have the occupiers consent
- under the practice address. When registering the patient, enter the full address, including postcode for the GP practice, putting ‘Care of’ at the start of the address. Writing ‘no fixed abode’ in any field will cause
- the registration request to be rejected.
Ensure that patients are advised to regularly check for post at the address they are registered at, so as not to miss any important medical correspondence (e.g. secondary care appointments).
Duty to refer
The Homelessness Reduction Act (2017) came into force in 2018. It places renewed emphasis on homelessness prevention. Section 10 requires public authorities in England to notify a local housing authority (LHA) of service users they think may be homeless or at risk of becoming homeless.
This statutory duty to refer applies to:
- NHS organisations that provide inpatient care
- emergency departments
- urgent treatment centres.
It is not mandatory for primary care providers. However, it is still beneficial for GP practices to refer patients who are homeless, or are at risk of becoming homeless, to a local housing authority for further support.
Referrals must include:
- the service user name
- their contact details and
- an agreed reason for referring the user.
You can refer without consent to safeguard children and vulnerable adults. Guidance on the duty to refer can be found here.
Patients About to be Released from Prison
The process for registering patients prior to their release from the “secure residential estate” which includes prison, immigration removal centres, young offender institutions or secure training centres, is outlined here.
Veterans
Ex-service personnel or reservists will be provided with copies of their medical records by DPHC (Defence Primary Health Care) on leaving the Armed Forces and becoming a veteran. These records should be given to their new GP practice on registering.
Armed Forces veterans are entitled to priority treatment if their injury or condition came about because of their service (subject to clinical need). This is regardless of whether they receive a war pension. Further guidance can be found here and here.
When registering veterans, the following SNOMED code should be entered at the time of registration: Military veteran SCTID: 753651000000107. Having this code will enable access to specialist care or charity support as necessary for the patient.
Mental Capacity Act
If a person is unable to register because they are unable to make decisions about their care, registration can be done by:
- A relative
- The main carer
- A lasting power of attorney
- A person appointed by a court under the Mental Capacity Act
NHS Health Checks and New Patient Health Checks
All newly registered patients should be offered a New Patient Health Check. Some patients may also be entitled to an NHS Health Check. Please refer to the health check policy for further guidance.
Please also see below patient health questionnaires for people seeking asylum and refugees which can be shared during registration to improve efficiency and effectiveness of New Patient Health Checks.
Further Resources and Guidance
NHS guidance:
- How to register with a GP surgery
- Asylum seeker and refugee one-page registration guide
- Primary Medical Care Policy and Guidance Manual (PGM)
BMA support:
- Guidance on patient registration
- Toolkit for asylum seekers and refugees
PCSE support:
- PCSE guidance on registration
- PCSE contact details and enquiries form
CQC guidance:
- Registration mythbusters
- Registration of migrants, asylum seekers and refugees
- People experiencing homelessness
OHID
- Migrant Health Guide
Doctors of the World
- Safe Surgeries network
- Patient health questionnaires for refugees and people seeking asylum
Subject Access Request
Suggestions and Complaints
We are committed to provide best possible care. If however, you have suggestions for improving our service or have a complaint about any aspect of our service you may ask for a suggestion slip/complaints pack or ask to speak to the Assistant Practice Manager of the site.
How to Complain
We hope that most problems are sorted out easily and quickly. Often at the time they arise and with the person concerned. If your problem cannot be sorted out in this way and you wish to make a complaint, we would like you to let us know ASAP. This would be within a matter of days or at most a few weeks because this will enable us to establish what had happened more easily.
If it is not possible to do that, please let us have details of your complaint:
- Within 6months of the incident that caused the problem;
Or
- Within 6months of discovering that you have a problem, provided this is within 12months of the incident
Complaints should be addressed to the Practice Manager. Alternatively you may ask for an appointment with the Practice Manager in order to discuss your concerns. They will explain the complaints procedure to you and will make sure that your concerns are dealt with promptly.
What we shall do
- We may ask you to put your complaint in writing
- We will acknowledge your complaint within two working days
- We will investigate the cause of your complaint
- We will aim to resolve your problem within ten working days
We will then be able to offer you an explanation or a meeting. When we look into your complaint we shall aim to;
- Find out what happened and what went wrong
- Make it possible for you to discuss the problem with those concerned (if you would like this)
- Where appropriate make sure you receive an apology
- Identify the problem and take steps to make sure the problem doesn’t happen again
Complaining on behalf of someone else
Please note that we keep strictly to the rules of medical confidentiality. If you are complaining on behalf of someone else, we must have his/her signed consent / permission.
Veteran Friendly
Patient charter: our commitment to you as a veteran of the UK Armed Forces
The NHS is here to help improve your health and wellbeing and keep you mentally and physically well. It is also here to help you get better when you are ill and, when you cannot fully recover, to stay as well as you can until the end of your life.
This means that you can expect the following from our practice
- We will ask all patients if they have served in the UK Armed Forces (as a regular or reservist). If you have, we will note this in your medical record, with your permission.
- We will ask you to share details of your time in service to help us to assess the best support and treatment for you.
- The information you share will be kept confidential and we will always speak to you before sharing this with other services you may be referred to.
- You can make an appointment to see our clinical lead for veteran’s health. This person has a comprehensive understanding of the Armed Forces, health conditions linked to service, and the dedicated support you can access.
- The NHS has a duty to support the health commitments of the Armed Forces Covenant. This means that you will get priority treatment for any medical condition which has been caused by your service, subject to the clinical needs of other patients.
- We will let you know what choices are available for your care and treatment and help you to make informed decisions on what to do.
- Where appropriate and with your consent, we can refer you to dedicated veterans health services.
- If you need to be seen by another service, we will let them know you’re a veteran and make sure they have an understanding of your health and wellbeing needs, so you don’t have to keep repeating your ‘personal story’.
- We can give advice and support to your loved ones who may be affected by your health conditions.
- We will investigate any issues and complaints that you may have about your care. If you have any concerns about the services we offer, please speak to one of the practice team.
Top tips for veterans
- It is important to register with a GP, rather than wait until you need treatment. Visit the NHS website to find details of GP practices in your local area.
- If you’ve recently left the forces, it is important to give your GP the paperwork that your military medical centre gave you, including any medical records. This will help to make sure your military health record transfers to your NHS health record. This will also give your GP information on your health and ensure that any ongoing care and treatment is continued.
- Regardless of when you left the military, tell your GP that you’ve served in the UK Armed Forces. This will help your GP to better understand any military related health conditions that you may have and ensure that you are referred, where appropriate, to dedicated services for veterans.
- This includes the specialist mental and physical health services, Op COURAGE: The Veterans Mental Health and Wellbeing Service and the Veterans Trauma Network.
- When using these services, you will be able to speak to people who:
- understand the Armed Forces and military life
- are either from the Armed Forces community or highly experienced in working with serving personnel, reservists, veterans and their families
- will work with you to make sure you get the right type of specialist care, support, and treatment
- work closely with a range of organisations and charities, including military charities, to support your wider health and wellbeing needs.
- With your agreement, it can sometimes be helpful for your doctor to refer you to Armed Forces charities, such as SSAFA, the Royal British Legion, Combat Stress or Help for Heroes. They can often offer significant help and support, even if they do not all deliver healthcare.
- You may be worried about sharing information about your time in the Armed Forces. Please note that the NHS is bound by a confidentiality code of practice to ensure GPs, nurses and other people working within the NHS deliver a confidential service bound by law.
To find out more, please speak to our practice manager or one of our GPs or nurses.
More information on health services for the Armed Forces Community
